Altitudinal visual field defect – assessment and clinical significance
Acute onset altitudinal visual field defect usually results from ischaemic optic neuropathy and is a neuro-ophthalmological emergency.
Jane Murphy, medical student elective assignment (Cambridge University, jm2122@cam.ac.uk)
Introduction and aetiology
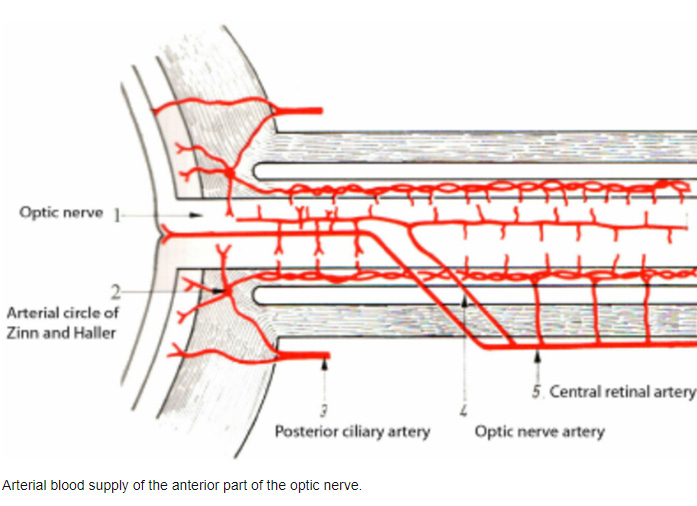
An altitudinal visual field defect (VFD) describes vision loss from the upper or lower part of the visual field without crossing the horizontal midline. Acute onset altitudinal VFD usually results from ischaemic optic neuropathy (ION), which is generally thought to affect one of the posterior ciliary arteries1,2. These arteries are part of the extracranial blood vessels, i.e. distal branches of the external carotid artery, and supply the superior and inferior segments of the anastomotic choroidal vascular bed. Ischaemia leads to infarctions in the corresponding part of the optic nerve head1,2, i.e. superior or inferior parts of the head of the optic nerve.
The aetiology of ION can be subdivided into arteritic – usually giant cell arteritis (GCA) – and non-arteritic, from shock or vasculopathy caused by cardiovascular risk factors such as hypertension, diabetes, hyperlipidaemia and smoking. In addition to ION, neuroinflammatory disorders are being increasingly appreciated as a cause of acute or subacute-onset altitudinal VFD. For example, it has been reported in episodes of optic neuritis from underlying neuromyelitis optica spectrum disorder (NMOSD)3–5. There are also case reports of altitudinal VFD in multiple sclerosis (MS)-related optic neuritis6–8, although central scotoma is much more prevalent. Gradual-onset altitudinal VFD is usually caused by open-angle glaucoma or optic disc drusen9. The wide variety of underlying aetiologies necessitates a detailed workup for any patient with an altitudinal VFD.
Patient case
Mr M is a 68-year-old gentleman with hypertension and diabetes who presented with blurred vision in his left eye. Mr M had woken up with this 2 days before the presentation, and it hadn’t significantly changed since that time. There were no other symptoms of note. Specifically, there was no fever, weight loss, periorbital pain, headache, scalp sensitivity or jaw claudication. Examination revealed a left-sided inferior altitudinal VFD with 6/6 corrected visual acuity, a relative afferent pupillary defect and normal eye movements. There was no palpable temporal artery or scalp sensitivity. Fundoscopy revealed hyperaemic papilloedema in the left eye. FBC, ESR and CRP were all within the normal range. A brain MRI revealed some small white matter hyperintensities on T2WI but was otherwise normal. Tonometry revealed normal eye pressure. Given the broadly normal investigations and patient risk factors, a diagnosis of non-arteritic ION was made.
History and examination
Time of onset:
As with most neurological presentations, acute onset suggests a vascular cause, subacute suggests inflammatory, and gradual suggests compressive, such as from a tumour or fluid buildup in glaucoma. A preceding episode of amaurosis fugax can occur in arteritic ION, and is rare in non-arteritic ION10.
Associated symptoms:
Periorbital pain, especially during eye movement, may indicate optic neuritis, as ION is characteristically painless.
Scalp sensitivity, jaw claudication and headache can point towards an arteritic ION.
Systemic features such as fever and weight loss may indicate giant cell arteritis or malignancy.
Examination
Acuity will reveal whether central vision is affected. It is often normal in altitudinal VFD.
Visual field testing to outline the extent of vision loss. In non-arteritic ION, inferior vision loss is much more common than superior11.
Reflex testing often reveals a relative afferent pupillary defect (RAPD).
Fundoscopy can reveal papilloedema in any cause of altitudinal VFD. A hyperemic disc suggests a non-arteritic ION or optic neuritis, whereas a pale disc tends to occur in arteritic ION, although this is not always the case.
Temporal artery palpation can reveal nodularity in GCA.
Ocular movement assessment.
Investigations
Bedside – blood pressure.
Bloods – FBC (thrombocytosis in GCA), ESR, CRP, HbA1c.
Imaging – Urgent CT head to rule out haemorrhagic and ischaemic stroke. MRI with contrast to identify space-occupying lesions and demyelinating lesions. MR angiography
Special tests – Optical coherence tomography, where you can measure peripapillary retinal nerve fibre layer (pRNFL) thickness, which is increased in ION and optic neuritis12 and can help differentiate MOGAD from MS13. Tonometry can be used to assess for glaucoma. Temporal artery biopsy is used to confirm suspected GCA.
Conclusion and outstanding questions
Determining the cause of a patient presenting with an altitudinal VFD is essential to direct the appropriate treatment. Arteritic ION requires urgent treatment with IV methylprednisolone and requires a high index of suspicion initially. Altitudinal VFDs impact skills such as driving and walking, reducing people’s quality of life and ability to function14. However, they can be overlooked because visual acuity is often spared. Public health measures to reduce the incidence and impact of these defects are required.
Questions remain around the pathophysiology of altitudinal VFDs. Whilst the vascular supply of the choroidal network explains the segmental nature of altitudinal VFD in ION, there is no current explanation for why optic neuritis leads to visual field defects that do not cross the horizontal midline. This may be related to the tendency of demyelinating lesions to centre on small venules, for example, in Dawson’s fingers. Further work is required to elucidate this, with potential implications for understanding and treating neuroinflammatory demyelinating disorders.
Author
Jane Murphy, 5th year medical student, Cambridge University (jm2122@cam.ac.uk)
Bibliography
1. Hayreh, S. S. Pathogenesis of visual field defects. Role of the ciliary circulation. Br. J. Ophthalmol. 54, 289–311 (1970).
2. Hayreh, S. S. In vivo choroidal circulation and its watershed zones. Eye 4, 273–289 (1990).
3. Nakajima, H. et al. Visual field defects of optic neuritis in neuromyelitis optica compared with multiple sclerosis. BMC Neurol. 10, 45 (2010).
4. Onder, H., Khasiyev, F. & Karabudak, R. Optic Neuritis Presenting With Altitudinal Visual Field Defect in a Neuromyelitis Optica Patient. J. Neurol. Res. 7, 112–114 (2017).
5. Liang, J. et al. Comparing evolvement of visual field defect in neuromyelitis optica spectrum disorder-optic neuritis and idiopathic optic neuritis: a prospective study. BMC Ophthalmol. 22, 338 (2022).
6. Akduman, R. C., Bayram, C., Calik, S. & Silek, H. Altitudinal Visual Defect as the Initial Sign of Optic Neuritis: A Case Report. J. Mult. Scler. Res. 2, 54–56 (2022).
7. Chin, C. W. & Ismail, M. F. Atypical presentation of optic neuritis with unilateral inferior altitudinal visual field defect in multiple sclerosis. Ophthalmol. J. 5, 130–135 (2020).
8. Abro, A. A., Falamarzi, A. & Shaikh, M. Y. Unilateral Acute Idiopathic Optic Neuritis With Superior Altitudinal Visual Field Defect as a Presenting Feature. Cureus (2021) doi:10.7759/cureus.17011.
9. Khan, K., Almarzouqi, S. J., Morgan, M. L. & Lee, A. G. Altitudinal Visual Field Defects. in Encyclopedia of Ophthalmology (eds. Schmidt-Erfurth, U. & Kohnen, T.) 74–74 (Springer Berlin Heidelberg, Berlin, Heidelberg, 2018). doi:10.1007/978-3-540-69000-9_1155.
10. Hayreh, S. S. Anterior ischaemic optic neuropathy Differentiation of arteritic from non-arteritic type and its management. Eye 4, 25–41 (1990).
11. Hayreh, S. S. Visual Field Abnormalities in Nonarteritic Anterior Ischemic Optic Neuropathy: Their Pattern and Prevalence at Initial Examination. Arch. Ophthalmol. 123, 1554 (2005).
12. Razaghi, G. et al. Measurement of retinal nerve fiber layer thickness with a deep learning algorithm in ischemic optic neuropathy and optic neuritis. Sci. Rep. 12, 17109 (2022).
13. Chen, J. J. et al. OCT retinal nerve fiber layer thickness differentiates acute optic neuritis from MOG antibody-associated disease and Multiple Sclerosis. Mult. Scler. Relat. Disord. 58, 103525 (2022).
14. Qiu, M., Wang, S. Y., Singh, K. & Lin, S. C. Association between Visual Field Defects and Quality of Life in the United States. Ophthalmology 121, 733–740 (2014).
15. Keltner, J. L. Visual Field Profile of Optic Neuritis: A Final Follow-up Report From the Optic Neuritis Treatment Trial From Baseline Through 15 Years. Arch. Ophthalmol. 128, 330 (2010).
16. Sharma, A., Kudchadkar, U., Shirodkar, R., Usgaonkar, U. S. & Naik, A. Unilateral inferior altitudinal visual field defect related to COVID-19. Indian J. Ophthalmol. 69, 989 (2021).




Hi Gavin
Is this the same.
The top left of my visual field deviation as consistently gotten more dots the print out for the past year. It only had two a year ago and now that top left corner is full of black dots on the visual field test.
The optic nerve mri has been said to “normal” despite one comment on their about possible thickening. Neuro-ophthalmology are saying it’s not ms. Ophthalmology alone are saying it’s concerning how much it’s gotten worse and they don’t understand why neuro-op aren’t “excited” by seeing this (in their words).
What does it sound like to you?