Hoover's sign
Level 1:
Hoover’s sign of leg paresis is one of two signs named after Charles Franklin Hoover (1865–1927), an American physician, born in Cleveland, Ohio, who studied medicine at Harvard.
The manoeuvre is aimed to separate organic or non-functional from non-organic or functional paresis of the leg. The sign relies on the principle of synergistic contraction of muscle groups. Involuntary extension of the "paralysed" leg occurs when flexing the contralateral leg against resistance.
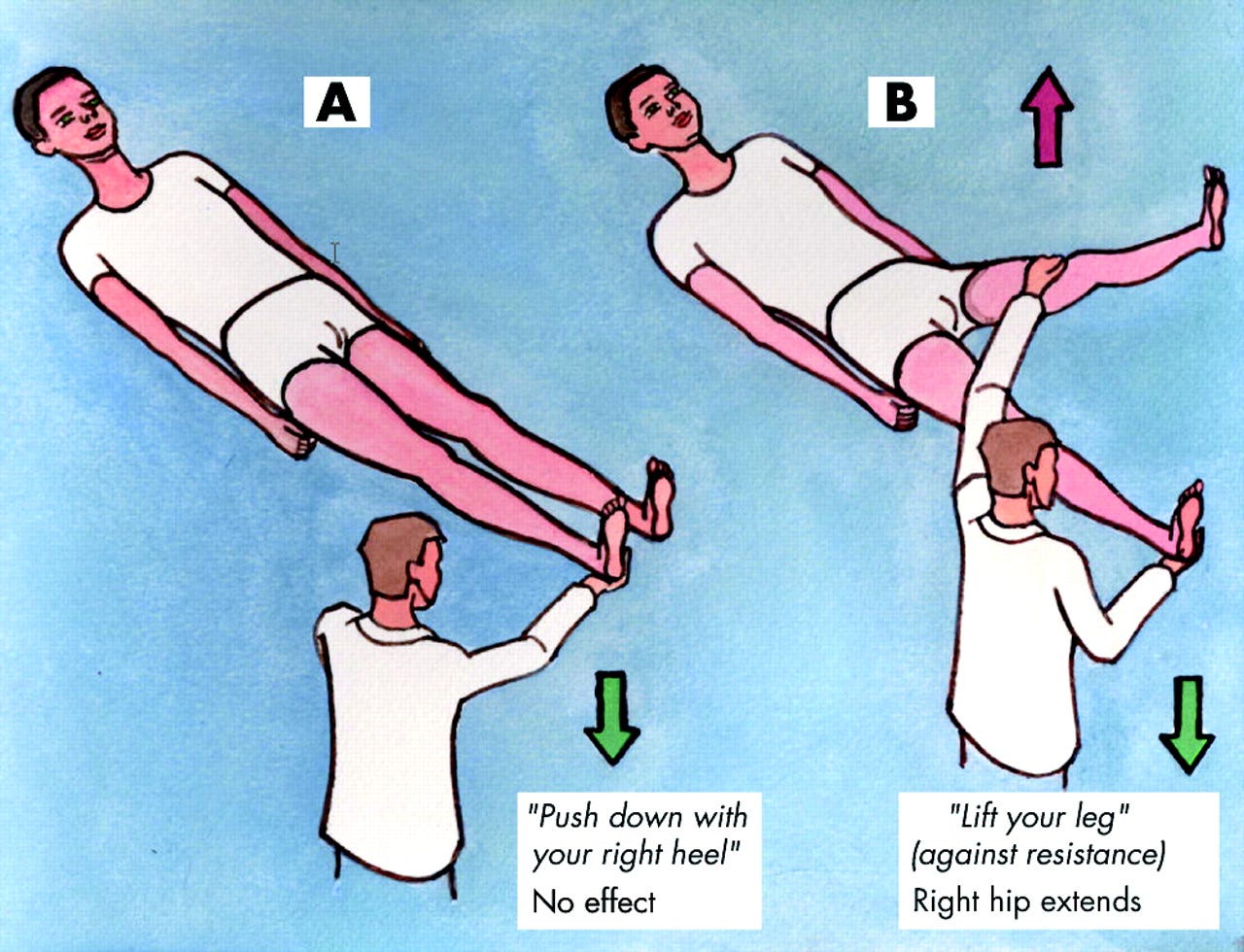
The figure below explains the principles of the test. If the patient has weakness when you test extension of the right leg (A) but has detectable power in the right leg when you test flexion of the left leg (B) it implies that the patient is likely suffering from non-organic limb weakness (positive Hoover's sign). In B the extension of the right leg occurs due to involuntary contraction of synergistic muscles.
I find a positive Hoover's sign a very useful clinical test to confirm a clinical suspicion of non-organic or medically unexplained symptoms. Please remember that a large number of patients may still have a organic disease despite a positive Hoover's sign; patients often try to enhance, or exaggerate, their symptoms and signs to make you take their complaints seriously; the medical jargon for this is "functional overlay". The diagnosis of medically unexplained symptoms is often very difficult; please don't rush to make this diagnosis particularly if you have any doubts.
For those of you doing general medicine a positive Hoover’s sign may refer to inward movement of the lower rib cage during inspiration, implying a flat, but functioning, diaphragm. This is typically associated with hyperexpansion of the lungs due to air trapping, particularly emphysema. The flattened diaphragm contracts inwards instead of downwards, thereby paradoxically pulling the inferior ribs inwards with its movement.
Source and further reading: Stone et al. Functional symptoms and signs in neurology: assessment and diagnosis. J Neurol Neurosurg Psychiatry 2005;76:i2-i12 doi:10.1136/jnnp.2004.061655


