What is the cortical syndrome?
He was making simple calculation errors with a task he had been doing for years.
Case study
A 26 year-male with multiple sclerosis is noticed to be acting strangely at work. Some of his colleagues saw he was making simple calculation errors with a task he had been doing for years. On his way to work that morning, he had problems using his bicycle, i.e. he could not use the bicycle gears and brakes correctly. He was taken to A&E, where he saw a neurologist. He was unable to write or do simple calculations, had left-right confusion and in the notes, it stated he had motor apraxia; i.e. he was able to explain how to use his bicycle’s breaks and gears but was unable to execute it with his hands when attempting to cycle.
What is the syndromic diagnosis?
What hemisphere and cortical region is involved?
What other clinical signs would you look for?
What feature is not part of this classic syndrome?
How would you test for left-right confusion?
What is motor apraxia?
How would you investigate this patient, and what is the most likely cause?
Case study answers
What is the syndromic diagnosis?
Gerstmann syndrome is a neuropsychological disorder characterised by the tetrad of (a) agraphia (inability to write), (b) acalculia (inability to perform mathematical calculations), (c) finger agnosia (inability to name, discriminate, or identify fingers), and (d) left-right disorientation (inability to distinguish left from right).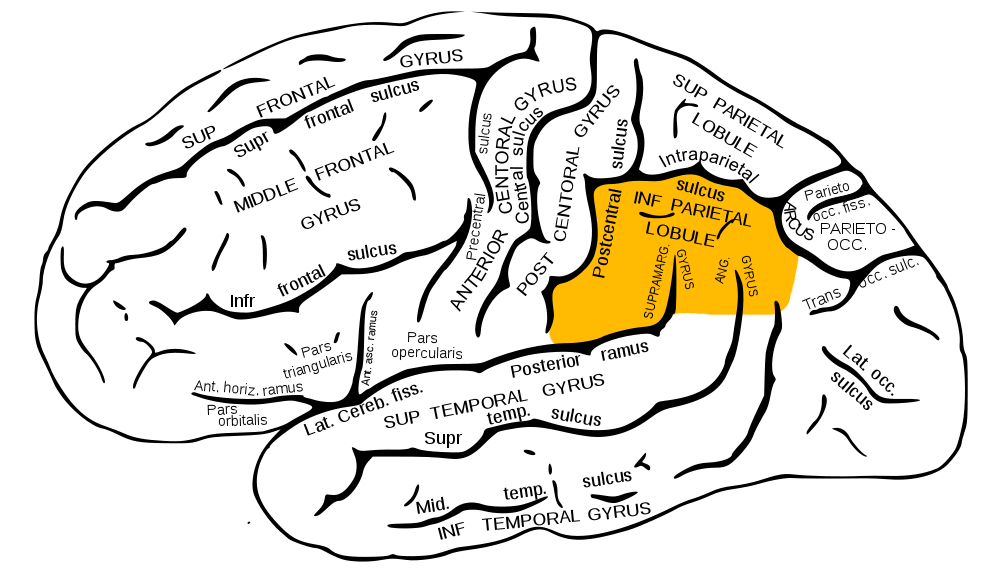
The inferior parietal lobule, with damage in this area most often associated with Gerstmann syndrome (Image from Wikipedia) What hemisphere and cortical region is involved?
Gerstmann's syndrome results from damage to the dominant (usually left) parietal lobe in the angular gyrus region.What other clinical signs would you look for?
Finger agnosia. Finger agnosia is the loss in the ability to distinguish, name, or recognise the fingers—not only the patient's fingers, but also the fingers of others, and drawings and other representations of fingers.What feature is not part of this classic syndrome?
Apraxia. Please note that this patient had ideomotor motor apraxia, indicating that more than the angular gyrus was involved, and the lesion extended into the posterior parietal lobe.How would you test for left-right confusion?
Left-right confusion or disorientation can be tested by asking the patient to show you their right and left hand and then to touch their left ear with their right hand and vice-versa. A positive test indicates the inability to obey these commands in the presence of otherwise normal sensory and motor faculties.What is motor apraxia?
Apraxia is an inability to correctly perform learned movements, even if the patient has relatively normal sensation and motor function. I like to think about it as a software problem, i.e. the basic hardware (sensory and motor function) is intact, but the brain can’t implement learned movements that they could do before. For example, in this case, he could not use the brakes and gears on his bicycle. The most involved body area usually classifies apraxia. Apraxia is considered one of the ‘higher cortical’ abnormalities in neurology.
Apraxia can be classified as follows:Ideational apraxia is when there is a failure to conceive or formulate a series of acts, either spontaneously or to command. For example, when writing and sending a letter, the patient with apraxia may seal the envelope before inserting the letter.
Ideomotor apraxia is when the patient may know and remember the planned action but cannot execute it with either hand (e.g., cutting a piece of paper with scissors).
Conduction apraxia is when the patient shows a more significant impairment when imitating movements than when pantomiming to command.
Disassociation apraxia is when the patient cannot usually gesture to command but can perform well with imitation and actual tools and objects.
Conceptual apraxia is when the patient makes content- and tool-selection errors. For example, when asked to demonstrate the use of a screwdriver, the patient may use it as if it were a hammer.
Please note that the term can be extended to specific tasks, for example, gait apraxia (see video below). Gait apraxia or frontal lobe gait apraxia is due to the involvement of the frontal lobe gait centres in the medial supplementary motor cortex. The important thing is that a patient with gait apraxia needs to have a relatively intact sensory and motor system; hence, the abnormality is referred to as apraxia, i.e. failure of a learned task, rather than due to weakness, incoordination or sensory/proprioceptive loss.
How would you investigate this patient, and what is the most likely cause?
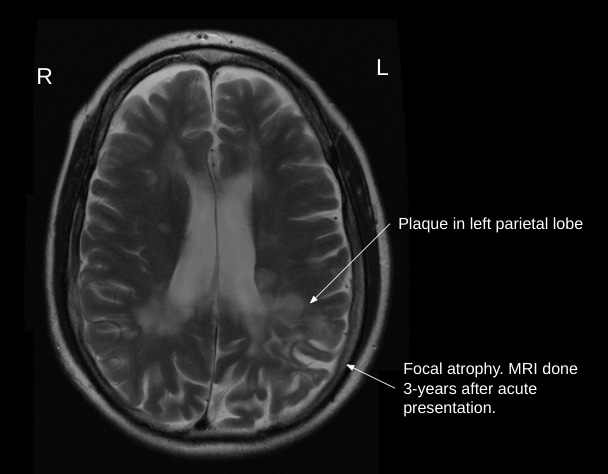
This patient needs brain imaging, ideally an MRI, as he has MS. Still, a CT scan would be sufficient to rule out a vascular lesion (infarct or haemorrhage), tumour or another space-occupying lesion (e.g. abscess). This patient would have needed a systemic work-up to look for signs of cardiovascular disease. A stroke in the middle cerebral artery territory is the most common cause of a dominant parietal lobe syndrome.
This patient turned out to have a sizeable demyelinating lesion in the left parietal lobe due to active MS. Please note that pure cortical syndromes are relatively uncommon presentations in MS. This patient was treated with high-dose methylprednisolone and subsequently was started on natalizumab for his multiple sclerosis. He made a relatively good recovery from his relapse, however, when the cause of the dominant parietal lobe syndrome is a stroke, the recovery is often poor.
Extra reading
E. Cubo, C.G. Goetz, Apraxia in Encyclopedia of the Neurological Sciences (Second Edition), 2014.
Ideomotor apraxia - https://en.wikipedia.org/wiki/Ideomotor_apraxia
Finger agnosia - https://en.wikipedia.org/wiki/Finger_agnosia
Gerstmann syndrome - https://en.wikipedia.org/wiki/Gerstmann_syndrome
General Disclaimer: Please note that the opinions expressed here are those of Professor Giovannoni and do not necessarily reflect the positions of Barts and The London School of Medicine and Dentistry nor Barts Health NHS Trust.